Clinical Program

About us
We are an ACGME accredited program that accepts four categorical residents per year. The program is five years in length with four and a half years spent at Cedars-Sinai (including three months at affiliate Kerlan-Jobe Institute for sports medicine), three months at Children's Hospital Los Angeles, and three months at Shriners Hospital for Children Los Angeles.
Click here to see access the Cedars-Sinai Graduate Medical Education website
Our clinical sites
The majority of the clinical rotations take place at Cedars-Sinai Medical Center, allowing the residents to easily attend all conferences. The hospital provides superb on-call facilities, excellent staff and ancillary services including a magnet nursing program, a dedicated orthopaedic surgical floor, around the clock intravenous, phlebotomy, and blood gas teams, EKG services, radiology technicians, and patient transport services.
Resident benefits
Competitive salary
Housing stipend of $12,000 per year
Educational stipend of $2000 per year
Fertility, preservation, assisted reproduction, adoption and gestational surrogacy care and services
Quarterly food allowances
Free parking
4 weeks of vacation per year
Sponsorship to attend and present original research at local, national and international conferences
Personal lead aprons and lead goggles
Reimbursement for educational expenses such as the DEA license, medical licensing, and Step 3
BLS, ACLS, and ATLS certification
*See additional benefit details on our GME website
Curriculum
Residents develop their surgical skills throughout residency training with early OR experience as PGY1s and increasing autonomy over time. They experience high surgical volume in all orthopaedic subspecialities and a wide spectrum of cases. The patient population at Cedars-Sinai is diverse, ranging from indigent, uninsured individuals to rare, complex orthopaedic referrals. Our faculty have decades of collective experience in residency education and are passionate about teaching. At Cedars-Sinai, residents benefit from mentorship, didactic instruction, and clinical experiences with these nationally renowned experts. All clinical rotations are accompanied by corresponding outpatient experiences, to enable the resident to be involved in the preoperative and postoperative phases of patient care. PGY5 residents are responsible for running the Orthopaedic Academic Clinic. All outpatient experiences are supervised by faculty.
Josh and John perform on total knee arthroplasty on Sawbones
PGY-1
Six months of General Surgery
Surgical Oncology
Vascular Surgery
General Surgery Night Float
Acute Care / Trauma Surgery, Surgical Intensive Care
Plastics and Reconstructive Surgery
Six months of Orthopaedic Surgery
Four months of Orthopaedic Trauma
Two months of Hand
One month of Musculoskeletal Radiology/Pediatric Orthopaedics
*Interns do not take in-house overnight call when they are on their Orthopaedic Trauma or Hand services. Interns are part of the General Surgery in-house overnight call pool on their General Surgery rotations.
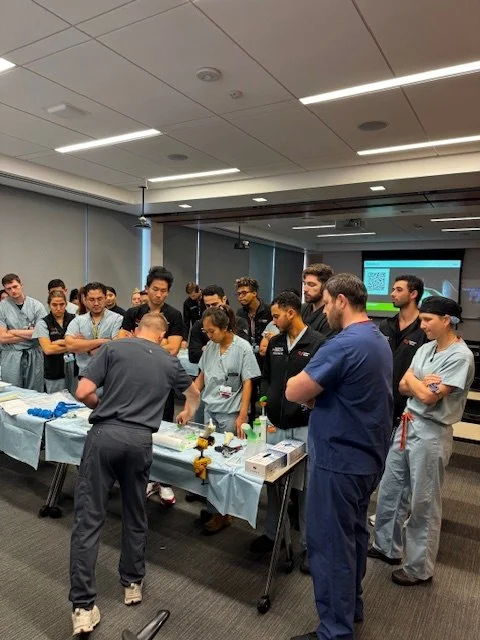
Tonya (right) leads a foot and ankle anatomy session for the residency group
PGY-2
Two month rotation blocks consisting of:
Orthopaedic Trauma (three blocks)
Spine surgery
Adult Reconstruction
Foot and Ankle
Second year residents will also take in-house overnight call approximately every fourth night. Post-call days are strictly protected.
PGY-3
Three month rotation blocks consisting of:
Sports Medicine (Kerlan-Jobe Institute/Santa Monica Orthopedic Group)
Adult Reconstruction
Orthopaedic Trauma
Pediatrics (Children’s Hospital of Los Angeles)
Third year residents cover operative weekend call (home call). Approximately 10-11 weekends per year.
PGY-4
Team Heal Football Game, PGY 4 Jalen Dansby assessing an injured player
Team Heal Jalen and Dr. Clarence Shields
Friday night lights, football game coverage. Johnny, Dr. Lerebours, Raj, Dr. Clarence Shields (former team doc of the LA Rams)
Two-three month rotation blocks consisting of:
Pediatrics (Shriners Hospital for Children Los Angeles)
Foot and Ankle
Orthopaedic Oncology
Spine surgery
Hand and upper extremity surgery
Fourth year residents act as chief residents taking home call every 8-10 days and 10 weekends throughout the year.
PGY-5
Orthopaedic Trauma (three months)
Adult Reconstruction (two months)
Sports Medicine (two months)
Elective (three months)
Research (two months)
Chief residents will also take home operative/chief call approximately every eight days.
Hands on cadaveric lab using robotic navigation
Didactics
The Didactic Education Program is designed to cover all aspects of orthopaedic surgery. Wednesday and Friday mornings are protected didactic time for residents, consisting of one hour attending led topical lectures and one hour of review lectures presented by senior residents. All senior residents (PGY4 and PGY5) play a significant role in teaching their peers and juniors. An additional hour is dedicated to a rotating schedule of cadaveric prosection, skills lab sessions in the Cedars-Sinai simulation center, monthly resident meetings, and additional critical topics such as practice management, medicolegal issues, and financial planning.
Skills lab sessions at Cedars-Sinai feature hands-on activities with representatives and equipment from a variety of vendors and equipment including robotic navigation, arthroplasty implants and sawbones. These opportunities allow residents to practice with the instrumentation and hardware they will experience in the OR.
Additional Educational Activities
The Department of Surgery has recently opened a Surgical Simulator Laboratory with advanced computerized simulators for arthroscopic surgery. Residents spend time in the facility under the guidance of faculty members. This laboratory is part of our sports medicine curriculum, designed to provide all residents with an appropriate experience in a wide range of arthroscopic procedures.
Biannual anatomy and skills labs are held at the DePuy Synthes laboratory site in Irvine, California. Residents work in pairs to perform entire upper and lower extremity dissections on fresh cadavers with faculty direction. These sessions are rare opportunities to practice surgical exposures, dissection technique and select procedures. Additional smaller anatomic dissection labs are held locally as well.
All PGY-2 residents are sponsored by the residency program to attend the AO Basic trauma course. All Cedars-Sinai trauma attendings are instructors at AO and Orthopaedic Trauma Association (OTA) courses. In addition to learning the fundamentals of fracture fixation and acute management, residents enjoy a wonderful social opportunity with their peers and attendings outside of the hospital.
In accordance with ACGME requirements, the program provides specific training on patient safety and ethical topics throughout the PGY1 year. These small group sessions are led by Dr. Paiement and often involving home-cooked meals at his house!
Daniel, Andrew, Maveric, Christian and Omar Learning about pelvic injuries at AO Basic. La Jolla, CA. 2025
All PGY-3 residents are sponsored by the residency program in partnership with industry to attend the Annual AAOS/AAHKS Fundamentals of Hip and Knee Arthroplasty meeting http://meeting.aahks.org/aahks-courses/resident-arthroplasty-course/.
All PGY-4 residents are sponsored by the program to attend the annual AAOS meeting for fellowship interviews, career networking and professional development.
Residents with specific interests have also attended the AO Advanced trauma course, Depuy Synthes Arthroplasty course, Medtronic Spine course, etc. supported by the department or industry grants. Funding and time away to attend additional courses is considered on an individual basis.
Departmental Education Activities
*Wednesday Morning Conference (7:00 a.m.):
Orthopaedic Grand Rounds three times per month
Monthly Morbidity and Mortality (M&M) conference
Quarterly Musculoskeletal Radiology/Orthopaedic Surgery combined conference
*Grand Rounds: These academic conferences are presented by departmental faculty or by nationally and internationally-renowned visiting professors. Previous invited speakers have included Dr. Douglas Dennis from University of Colorado (Joints), Dr. David Helfet from HSS Chief Emeritus (Trauma/Adult Reconstruction), and Dr. Amy Ladd of Stanford (Hand Surgery). This lecture series is designed to present cutting-edge research and contemporary clinical practices. Residents are exempt from clinical duties during the conference and have the opportunity for additional small group case presentations with the guest speakers.
*Core Curriculum: Wednesday’s from 8:00-9:00am and Friday’s from 7:00–9:00 a.m. This is a weekly protected block for resident education involving one hour didactic lectures by attending faculty. The remaining time is reserved for additional educational endeavors such as question review for the Orthopaedic In-Training Exam (OITE), cadaveric dissections, saw-bones workshops, surgical skills labs, etc.
Dr. Tsai teaching our new interns how to suture
Cementing lab led by Dr. Polakof and Dr. Burr
Service Specific Educational Activities
Trauma
Trauma Pass-On Rounds with all trauma attending faulty, daily, 6:30–7:00 a.m.
Combined Plastic Surgery and Orthopaedic Trauma Case Review and Fracture Conference, Tuesdays, 7:00–8:30 a.m. (A case-based conference and focused review of all surgical cases from the prior week)
Orthopaedic Trauma Didactic Teaching & Walk Rounds, Thursday, 7:00–8:00 a.m.
Arthroplasty
Didactics, Thursday, 9:00–10:00 a.m.
Arthroplasty Conference, Tuesday, 6:30 a.m. (A case-based conference as well as a forum for practice with the oral examination format)
Arthroplasty research meeting, 1st and 3rd Wednesday of each month, 6:30 am
Spine
Spine Conference, Wednesday, 7:00–8:00 a.m. (Features grand rounds presentations and case-based discussions)
Foot & Ankle
Foot & Ankle Conference, Tuesday, 7:00-8:00 am
Hand
Hand Surgery Teaching Conference, Monday, 5:00–6:00 p.m.
Hand Surgery AAOS Core Curriculum, Thursday, 5:00 p.m.
Sports
Sports Lectures, Thursday pm.
In addition, there are a number of special lectures throughout the year organized by the Department of Surgery and other medical divisions.
All residents are required to take the Orthopaedic Surgery In-Training Examination (OITE) every year and undergo year-around preparation through AAOS ResStudy and Orthobullets.